Gastrointestinal (GI) Disease Diagnostics

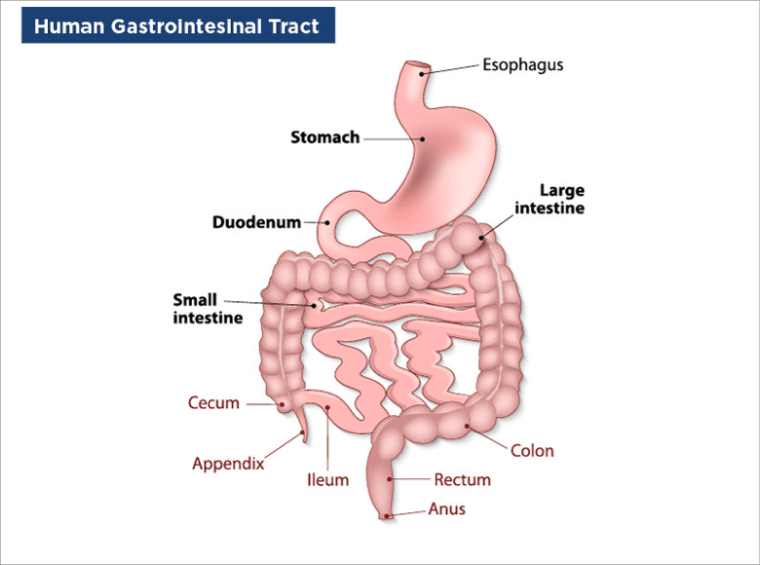
Gastrointestinal (GI) diseases, sometimes referred to as digestive diseases, are health problems that occur in the digestive tract. GI disorders can affect us in many ways, and they comprise a broad-spectrum of functional, inflammatory, and cancerous disorders of the digestive tract (esophagus, stomach, small intestine, large intestine, and rectum) and accessory organs of digestion such as the liver, gall bladder, and pancreas. Conditions may range from mild to serious to life threatening. This topic will review some of the most common GI diseases and their diagnostics. Gstrointestinal disorders represent a significant global health burden and encompass a broad spectrum of functional, inflammatory, and neoplastic conditions.
Symptoms of Gastrointestinal (GI) Diseases
The signs and symptoms of GI diseases vary considerably because of the location in the GI tract, the severity of the condition, and the underlying pathophysiology. Patients may have symptoms related to the digestive system, symptoms affecting other parts of the body, or no symptoms at all. Symptoms are often non-specific and may overlap across different gastrointestinal conditions, requiring careful clinical and laboratory evaluation. The first sign of problems in the digestive tract often includes one or more of the following symptoms:
- Bleeding
- Bloating/flatulence
- Constipation
- Diarrhea
- Heartburn
- Incontinence
- Nausea and vomiting
- Stomach pain
- Swallowing difficulties
- Weight gain or loss
Classifying Types of Gastrointestinal (GI) Diseases
Gastrointestinal disorders can be broadly categorized based on their underlying pathophysiology. GI diseases typically fall into one of three groups:
- Functional Gastrointestinal Disorders (FGIDs)
- Inflammatory Bowel Disease (IBD)
- GI Cancers
Functional Gastrointestinal Disorders (FGIDs)
Functional gastrointestinal disorders (FGIDs) are some of the most frequent reasons for us to visit physicians. They are common disorders that are characterized by persistent and recurring GI symptoms and they occur as a result of abnormal functioning of the GI tract.
Irritable Bowel Syndrome (IBS), which is characterized by abdominal pain associated with diarrhea, constipation, or alternating between both, is the most common FGID, while others include functional dyspepsia (pain or discomfort in the upper abdominal area, feeling of fullness, bloating, or nausea), functional vomiting, functional abdominal pain, and functional constipation or diarrhea.
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) describes disorders of the gut in which the intestines become inflamed. There are 2 major types of IBD: ulcerative colitis and Crohn's disease. Ulcerative colitis is limited to the colon or large intestine while Crohn's disease can involve any part of the GI tract from the mouth to the anus. Most commonly, it affects the last segments of the small intestine or colon or both.
IBD usually has a waxing and waning course. When there is severe inflammation, the disease is considered active, and a patient will experience a flare-up of symptoms. When there is less or no inflammation the disease is said to be in remission and the patient will not have any symptoms.
Celiac disease is another inflammatory disorder that people with a genetic predisposition experience with the ingestion of gluten (a protein found in wheat, barley, and rye) an immune reaction that primarily affects the small intestine.1
Poor Clinical response
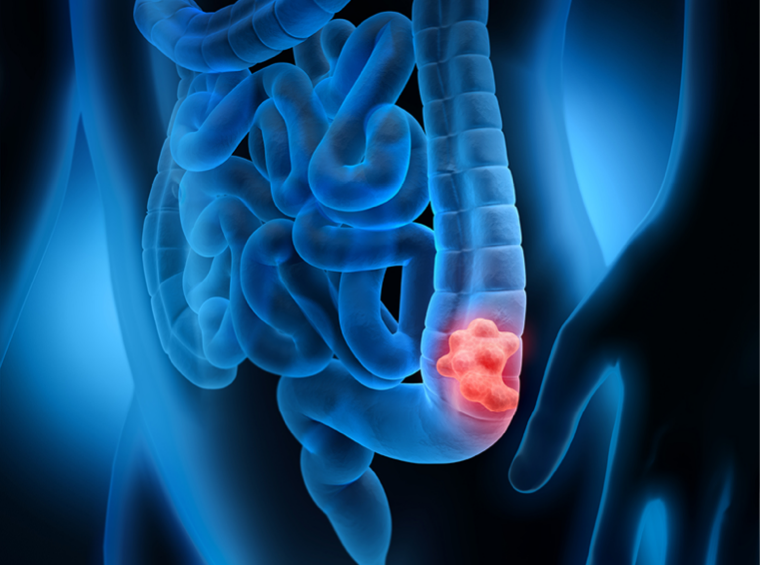
GI cancers are a group of cancers that affect the digestive system, and they include cancers of the esophagus, stomach, small intestine, bowel (large intestine or colon and rectum), anus, gallbladder, liver, and pancreas.
Epidemiology of Gastrointestinal (GI) Diseases
There are global variations in the prevalence of many gastrointestinal disorders because of differences in diets, sanitation, genetics, and environmental exposure. As developing countries become more affluent, these differences will likely start to reduce.²
FGIDs represented by functional dyspepsia (FD) and irritable bowel syndrome (IBS) are a group of disorders that include variable combinations of chronic or recurrent GI symptoms not explained by structural or biochemical abnormalities. FGIDs account for a significant number of patient visits to physicians. Although the definition of FGIDs can affect reported prevalence rates, the rates of FD and IBS diagnosed by the Rome III criteria in the general population were between 5.3 and 20.4% and 1.1 and 29.2%, respectively.³ The prevalence of IBD increased substantially in many regions of the world from 1990 to 2017. In 2017, there were 6.8 million (95% UI 6,4–7,3) cases of IBD globally. The age-standardized prevalence rate increased from 79.5/100.000 population in 1990 to 84.3/100.000 population in 2017. At a regional level, the highest age-standardized prevalence rate in 2017 occurred in high-income North America (422.0/100.000) and the lowest age-standardized prevalence rate was in the Caribbean (6.7/100.000 population).⁴⁻⁵
Cancers in the digestive system are a common cause of morbidity and mortality. In the 2018 IHME, Global Burden of Disease Collaborative Study, colorectal cancer was the third most prevalent cancer (affecting 9.35 million people worldwide: 0.12% of the world's population). Rates for other digestive system cancers were stomach (2.82 million people; 0.04%), esophagus (0.806 million people; 0.01%), liver (0.803 million people; 0.01%), and pancreas (0.381 million people; <0.01%). The epidemiology of gastrointestinal disorders varies by geographic region, age group, and underlying risk factors.
Diagnostics for Gastrointestinal (GI) Diseases
Alteration in bowel habits and abdominal pain are common symptoms in the general population, and differentiation between organic bowel disorders and FGIDs therefore represents a major challenge for physicians. Laboratory testing plays a central role in the differential diagnosis, risk stratification, and monitoring of gastrointestinal disorders. Confirmatory diagnosis generally involves a comprehensive analysis of clinical findings, serological findings, radiological imaging, invasive endoscopy, and histopathological examination. The selection of patients who should undergo radiological and/or endoscopic procedures, which are costly and invasive, is an important consideration, but needs to be balanced against the underestimation of potentially dangerous diseases such as colorectal cancer. The identification and use of specific biomarkers for different GI diseases would be a large step in the right direction.

Calprotectin is a protein released by neutrophils (a type of white blood cell) when the GI tract is inflamed, including inflammation caused by IBD. Thus, elevated fecal calprotectin levels are indicative of intestinal inflammation, including inflammation caused by IBD. Therefore, it helps to differentiate FGDIs from IBD. In patients with Crohn's disease or ulcerative colitis, fecal levels of calprotectin correlated closely with fecal excretion of indium-labelled leukocytes and is considered to be a benchmark for estimating intestinal inflammation.
Scientific materials
References
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet 2018; 391:70–81. PUBMED Link.
- Menon R, Riera A, Ahmad A. A global perspective on gastrointestinal diseases. Gastroenterol Clin North Am. 2011 Jun; 40(2):427-39. PUBMED Link.
- Oshima T, Miwa H. Epidemiology of Functional Gastrointestinal Disorders in Japan and in the World. J Neurogastroenterol Motil. 2015 Jul 30; 21(3):320-9. PUBMED Link.
- GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020; 5(1):17-30. PUBMED Link.
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, United States: The Lancet; 2018. Link.