Other Autoimmune Diseases

Other Autoimmune Diseases
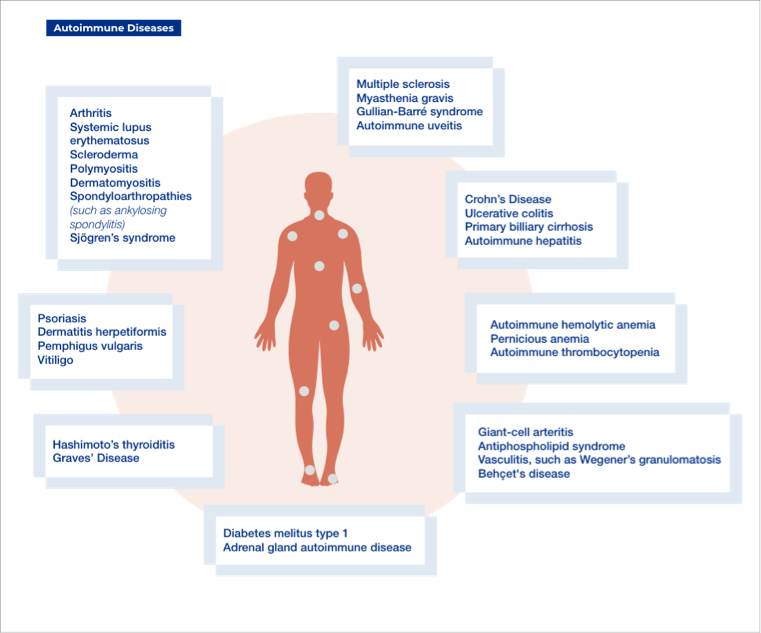
Autoimmune diseases are caused when the immune system mistakenly attacks itself. They affect 3–5% of the population and include common diseases (e.g. type 1 diabetes, rheumatoid arthritis, and psoriasis) and very rare diseases (e.g. Goodpasture syndrome). Although what causes autoimmune diseases is not entirely certain, genetic susceptibility and environmental factors (e.g. diet, exposure to toxic chemicals or metals, and infections) are thought to play a key role in the development of these diseases.¹ Recently, vitamin D deficiency has also been linked with various autoimmune diseases.² This article will review the symptoms, treatments and other important factors for a range of autoimmune diseases.
Vitamin D and Autoimmune Diseases
Appropriate levels of vitamin D are associated with general wellbeing. Vitamin D is available from food (vitamin D2 or ergocalciferol) or synthesized in the skin in response to exposure to sunlight (vitamin D3 or colecalciferol). Vitamin D2 and D3 are inactive forms of vitamin D, which are converted to the active form calcitriol by a two-step process in the liver and kidneys. Calcitriol plays an important role in regulating calcium and phosphorus levels in the body and maintaining healthy bones.³
Vitamin D can affect different types of tissues by suppressing cell growth, regulating cell death and controlling the activity of cells that carry vitamin D receptors (e.g. thyroid gland, reproductive tract, and the immune system).⁴ Vitamin D can modulate both innate (natural) and adaptive (acquired) immunity, and vitamin D deficiency is often seen in patients with autoimmune diseases although not everyone with vitamin D deficiency develops autoimmune diseases. Vitamin D deficiency is a risk factor only in people who are susceptible to autoimmune diseases such as type 1 diabetes, multiple sclerosis (MS), rheumatoid arthritis, and systemic lupus erythematosus (SLE). Vitamin D deficiency can also affect the symptoms and severity of these diseases.⁴
Sjögren's Syndrome
Sjögren's syndrome is a complex autoimmune inflammatory disease that causes dry mouth and dry eyes, as the glands that produce these fluids are damaged by immune system attack. Other symptoms include skin, nasal and vaginal dryness, swollen salivary glands, musculoskeletal pain, fatigue, and dysfunction of organs (e.g. kidneys and gastrointestinal system). Nine out of 10 cases of Sjögren's syndrome occur in women.⁵ Treatments to relieve symptoms and prevent complications include artificial tears for dry eyes, good oral hygiene and saliva substitutes for dry mouth, corticosteroids and hydroxychloroquine for arthritis, and biological agents (e.g. monoclonal antibodies) for severe inflammatory symptoms.⁶
Hashimoto's Thyroiditis
Hashimoto's thyroiditis is an autoimmune disease in which the thyroid gland is gradually destroyed. It is the most common cause of hypothyroidism (the thyroid gland is not able to produce enough thyroid hormone) in the United States and in regions of the world where iodine intake is inadequate. Early symptoms include constipation, fatigue, dry skin, and weight gain, which may be followed by cold intolerance, decreased sweating, and pressure symptoms in the neck from goiter (abnormal enlargement of the thyroid gland; e.g. voice hoarseness). There is no cure for Hashimoto's thyroiditis. Thyroid hormone replacement, usually with oral levothyroxine sodium, is the standard treatment for hypothyroidism.⁷
Graves' Disease
Graves' disease mainly affects the thyroid gland and may affect multiple other organs including the eyes and skin.⁸ It is the most common cause of hyperthyroidism (the thyroid gland produces too much thyroid hormone). The body's immune system is tricked into targeting receptors on the thyroid gland, causing hyperthyroidism. Research suggests that Graves' disease may be caused by a combination of genetic and environmental factors. It is caused by thyroid-stimulating immunoglobulin, which binds to thyroid-stimulating hormone receptors on the thyroid cell membrane and stimulates thyroid hormone synthesis and thyroid gland growth, causing hyperthyroidism and goiter. Younger patients may experience heat intolerance, sweating, fatigue, weight loss, and goiter. The elderly population may have non-specific symptoms such as fatigue, weight loss, and atrial fibrillation (irregular heartbeat). Treatment consists of reduction in thyroid hormone secretion by using antithyroid drugs, radioactive iodine, or total or partial thyroidectomy (removal of the thyroid gland).⁸
Idiopathic Thrombocytopenic Purpura (ITP)
Idiopathic thrombocytopenic purpura is an immune disorder in which the blood doesn't clot normally. ITP usually happens when the immune system mistakenly attacks and destroys platelets. Therefore there are few platelets in the blood (thrombocytopenia; platelet count <150,000/µL) due to platelet destruction and impaired platelet production, resulting in an increased risk of bleeding.¹¹⁻¹² Symptoms may include bruising, bleeding from the nose or mouth, bleeding into the skin (reddish-purple spots that look like rash), and abnormally heavy menstruation. Treatment is initiated when significant bleeding occurs. Corticosteroids (e.g. prednisone), intravenous immunoglobulin (IVIG), and anti-D immune globulin (in patients who have a Rh-positive blood type) are the first treatment options for quick recovery of platelet counts.¹²⁻¹³
Addison's Disease (AD)
Addison's disease (or primary adrenal insufficiency) is an uncommon condition that occurs when the body does not produce enough cortisol and aldosterone (hormones). It results from damage to the outermost layers of the adrenal gland (adrenal cortex). Most cases of Addison's disease result from a problem with the adrenal glands themselves (primary adrenal insufficiency). Autoimmune disease accounts for 70% of Addison's disease. This occurs when the body's immune system mistakenly attacks the adrenal glands. AD affects 40–60 people/million and occurs in equal numbers in men and women.¹⁰ Symptoms include fatigue, gastrointestinal abnormalities (e.g. nausea and vomiting), changes in skin color, low blood pressure (hypotension), dehydration, and depression. It is treated by replacing the missing hormones: cortisol is replaced by the drug hydrocortisone and aldosterone is replaced by the drug fludrocortisone.¹⁰ ¹⁴
Polymyositis (PM)
PM is chronic inflammation of the muscles (inflammatory myopathy) that causes progressive muscle weakness, largely affecting the shoulders, upper arms, pelvis, and thighs. Eventually, it becomes difficult to lift the arms, get out of a chair, or climb steps. If neck and throat muscles are affected, it can result in difficulty swallowing and cause changes in voice.¹⁰ In most cases, the cause of an inflammatory myopathy like polymyositis (PM) is unclear. The body's immune system turns against its own muscles and damages muscle tissue in an autoimmune process. Viruses might be a trigger for autoimmune myositis. It is most common in adults who are 45–60 years old, occurs twice as often in women than in men, and is more common in African Americans than Caucasians. PM is treated with corticosteroids (e.g. prednisone), immunosuppressive drugs (e.g. methotrexate and azathioprine), synthetic adrenocorticotropic hormone, and IVIG.¹⁰
Dermatomyositis (DM)
DM is a chronic inflammation of the muscles (inflammatory myopathy) that causes muscle weakness and skin rash.¹⁰ The body's immune system turns against its own muscles and damages muscle tissue. In most cases, the cause of an inflammatory myopathy is unclear. In dermatomyositis, cells attack the small blood vessels that supply muscles and skin. The main symptom is muscle weakness affecting the hips, thighs, shoulders, upper arms, and neck. Muscle weakness and muscle wasting (atrophy) progresses over time and eventually leads to difficulty walking, lifting arms, climbing steps, or dressing. A reddish-purple/lilac rash on the upper eyelids (heliotrope eyelids) or across the cheeks and bridge of the nose ("butterfly" rash) and on the forehead and scalp may also appear. It affects approximately 10 per million people and occurs twice as often in women than in men. DM is treated with corticosteroids (particularly prednisone), immunosuppressive drugs (e.g. methotrexate and azathioprine), and antimalarial drugs (e.g. hydroxychloroquine).¹⁰
Multiple Sclerosis (MS)
MS is a chronic inflammatory disease of the central nervous system (CNS; brain, spinal cord and optic nerves) that affects movement, sensation, and body functions. In MS, the immune system mistakenly attacks the protective layer around nerve cells (myelin sheath) in the brain, spinal cord, and optic nerves. The myelin sheath is also important for the transmission of nerve electrical impulses and scarring of the sheath (sclerosis), slows or blocks messages from the brain, resulting in problems with vision, balance, muscle control, and other basic bodily functions. As there is no cure for MS, treatment with disease-modifying drugs (e.g. beta-interferons and immunosuppressants) helps to reduce symptoms and prevent irreversible damage to the CNS. Physical, speech and occupational therapies, exercise, rest, and healthy nutrition may also help to relieve symptoms.¹⁵⁻¹⁶
Sarcoidosis
Sarcoidosis is a chronic inflammatory disease which results in the growth of tiny collections of inflammatory cells (granulomas) in any part of the body, particularly the lungs and lymph nodes. Other organs (e.g. eyes, skin, nervous system and heart) may also be affected. Symptoms may vary depending on the affected organs, with fever, unintentional weight loss, and fatigue likely to occur in about one-third of patients, and shortness of breath, dry cough, and chest pain in about half of all patients. Sarcoidosis can be treated with corticosteroids (e.g. prednisone), immunosuppressants (e.g. methotrexate, azathioprine, and leflunomide) and biological agents (e.g. monoclonal antibodies).¹⁷
Scientific materials
References
- Wang, L., F. S. Wang and Gershwin M. E. Human autoimmune diseases: a comprehensive update. J Intern Med. 2015; 278(4): 369-395. PUBMED link
- Agmon-Levin, N., Theodor E., Segal R. M. and Shoenfeld Y. Vitamin D in systemic and organ-specific autoimmune diseases. Clin Rev Allergy Immunol .2013; 45(2): 256-266. PUBMED link
- Institute of Medicine (US) Committee. Overview of Vitamin D. En: A Catharine Ross, Christine L Taylor, Ann L Yaktine, and Heather B Del Valle Editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): The National Academies Press: 2011; Chapter 3. P.1-1115 PUBMED link
- Abumohor, P. Vitamin D and autoimmune diseases. In: IV Symposium on Autoimmunity - Present and future in the diagnosis and treatment of autoimmune disease. Santiago, Chile: Grifols, S.A.; 2018. Chapter 2, pp 8-15.
- Jisha J. Nair, Tejas P. Singh. Sjogren's syndrome: Review of the aetiology, Pathophysiology & Potential therapeutic interventions. J Clin Exp Dent. 2017; 9(4): e584-e589. PUBMED link
- Stefanski, A. L., C. Tomiak, U. Pleyer, T. Dietrich, G. R. Burmester and T. Dorner. The Diagnosis and Treatment of Sjogren's Syndrome. Dtsch Arztebl Int. 2017; 114(20): 354-361. PUBMED link
- Mincer, D. L. and I. Jialal. Hashimoto Thyroiditis. Treasure Island (FL): StatPearls [Internet]; 2020. Available at https://www.ncbi.nlm.nih.gov/books/NBK459262/ PUBMED link
- Pokhrel, B. and K. Bhusal. Graves Disease. Treasure Island (FL): StatPearls [Internet]; 2019. Available at: https://www.ncbi.nlm.nih.gov/books/NBK448195. PUBMED link
- Furuta S, Iwamoto T, Nakajima H. Update on eosinophilic granulomatosis with polyangiitis. Allergol Int .2019; 68(4): 430-436. PUBMED link
- New Maria I.,MD. Addison's Disease [Internet]. Mount Sinai School of Medicine: National Organization for Rare Disorders; 2019. [Accessed 3 Dec 2019]. Avaible at: https://rarediseases.org/rare-diseases/addisons-disease/ link
- Khan, M. and Mikhael J. A review of immune thrombocytopenic purpura: focus on the novel thrombopoietin agonists. J Blood Med. 2010; 1: 21-31. PUBMED link
- Zainal, A., A. Salama and Alweis R. Immune thrombocytopenic purpura. J Community Hosp Intern Med Perspect. 2019; 9(1): 59-61. PUBMED link
- Khan, A. M., H. Mydra and A. Nevarez. Clinical Practice Updates in the Management Of Immune Thrombocytopenia.P T. 2017; 42(12): 756-763. PUBMED link
- Burton, C., Cottrell E. and Edwards J. Addison's disease: identification and management in primary care. Br J Gen Pract. 2015; 65(638): 488-490. PUBMED link
- Goldenberg, M. M. Multiple sclerosis review. P T. 2012; 37(3): 175-184. PUBMED link
- Dobson, R. and Giovannoni G. Multiple sclerosis - a review. Eur J Neurol. 2019; 26(1):27-40. PUBMED link
- Soto-Gomez, N., Peters J. I. and Nambiar A. M. Diagnosis and Management of Sarcoidosis. Am Fam Physician. 2016; 93(10): 840-848. PUBMED link